Alison: I couldn’t be happier to kick off the New Year with this post from Denis Asselin, an amazing advocate who’s been working tirelessly and with compassion to spread awareness about body dysmorphic disorder (BDD) since his son, Nathaniel, committed suicide after struggling with the disorder for years.
We all know how misunderstood OCD is, and it’s possible BDD is even more misunderstood. Denis is working hard to change that. His dedication is inspiring — and, honestly, he is so nice. Incredibly, genuinely nice. You can’t help but want to help him tell Nathaniel’s story and join his cause.
Q. I’m always amazed to see what a parent is capable of after the tremendous pain of losing a child. After your son, Nathaniel, committed suicide you took action. Since 2012 you have participated in your initiative, “Walking With Nathaniel,” walking thousands of miles and raising thousands of dollars to spread awareness of the illness that led to Nathaniel’s death, BDD. Tell us why.
A. What does a parent do when s/he loses a child? Initially, cry a lot. What an incredibly sad event! Losing a child is the ultimate loss, and definitely not the natural order of things. The event and its repercussions were so significant. We were like ants at the base of Mt. Everest, required to climb to the very summit. I not only lost my personal and spiritual “equilibrium,” but initially I also lost a sense of purpose for living. As a father, I’m instinctively programmed to preserve and protect my children, and through no fault of my own, it felt as if I had failed in that critical mission. So what’s next when the void looms so large before you?
I distinctly remember seeing myself at a junction, the intersection of two possible paths to take for the rest of my life — one was to inevitably fold into myself, live in constant self-pity, be perpetually grumpy, and see myself as the ultimate victim. The energy required in the choice of that particular path would be dark, negative, and all-consuming. My social arena would close and include no one else; I would be a hermit and I would yell and blame everyone for everything, consider the universe totally unfair, and spread an aura of darkness wherever I found myself. The other road led to slow and progressive healing, to an eventual reordering of my life with what is (not what should have been). Bitterness would eventually melt away, and new possibilities would slowly reveal themselves and emerge. I would slowly see beauty and light pierce the huge darkness and recognize once again the gift of possible life and living before me, rather than a death in life. That vision/possibility included a forward movement — first in small steps and then in bigger ones. To me, walking forward reflected that outward expansion and healing.
After my wife, Judy, and my daughter, Carrie, and I returned from Spain where we had walked for three weeks on the Camino de Santiago after Nathaniel’s death, I felt as if I had more walk in me. Every time I took a step forward, I felt much better. At first I started to walk in circles (daily walks around the neighborhood) in wider and wider concentric circles. It was during those circular peregrinations that I hatched the plan to walk in a line rather than in a circle from our hometown (Cheyney, PA) to Boston, MA. I envisioned a new kind of “pilgrimage” à la El Camino, but here in the USA instead — a personal spiritual and physical journey of healing. I asked myself, “What would it look like to walk out my front door and go to Boston (the home of the International OCD Foundation), connecting along the way all the happy and sad chapters/places/events in Nathaniel’s life like dots on a trail map (where he was born, where he went to school, where he got his first job, where he died, where he was first hospitalized, where he stayed in clinics and treatment centers thereafter, where he had appointments with his doctors, psychiatrist, psychologists, and counselors)?” The imagined trajectory spanned 552 miles to Boston where he had spent an entire day in the Emergency Room at Mass General back in 2009 desperately seeking help because he couldn’t do “his life” anymore. I wanted my pilgrimage to end at the Boston harbor, at the water’s edge (just like Finisterre over the cliffs of the Atlantic in Spain at the end of the Camino). I would then face toward the east where the sun rises — again a symbol of an opening rather than a closure. That is how the Camino de Nathaniel was born and executed in 2012.
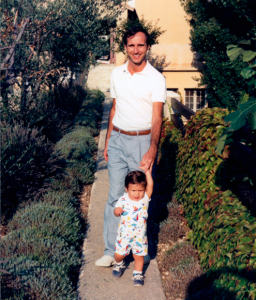
Denis walking with Nathaniel
Q. Tell us about Nathaniel. What kind of kid was he? What was he passionate about?
A. Nathaniel was an amazing human being. His spirit could fill the room, so could his physical presence — he was tall, handsome, fit, intelligent, highly responsible, sensitive, compassionate, loving, magnetic, funny, engaging, strong, athletic, generous, quick of mind, creative, energetic, positive, in brief a very old soul. I’m not saying this because he was my son. I recognized his incredible gifts and talents starting on the day he was born. He stared me in the eyes letting me know he was ready to journey forth. His close friends, Judy, Carrie, and extended family members would also describe him with the same litany of adjectives. Everyone loved Nathaniel. His force field was so strong. Everyone wanted to be his friend. Everyone wanted to be in his presence. Unfortunately, OCD/BDD slowly gnawed away at these incredible positive attributes during the long years of his illness. But even in the depth of his sickness, those deeply rooted qualities still radiated through in some recognizable measure. He was passionate about running, playing, and engaging in creative and imaginative games, staying fit, and doing his very best at all the time.
Q. When was Nathaniel diagnosed with BDD, and how did you realize something might be wrong?
A. Unfortunately, the BDD diagnosis came much later during his 13-year illness, when he was 17. He was hospitalized at 11 for OCD behavior (but somehow the diagnosis seemed incomplete and not totally accurate). Then we began to see him spend more and more time in the bathroom grooming himself, worrying about flab on his tummy (there was actually none there) and imagined dark circles under his eyes, the placement of his hair, and the quality of his skin (any marks on his face would ruin his day and keep him in the bathroom for hours picking at it). He spent less and less time with his friends and worried more and more about his appearance and looks. He would look away and avoided eye contact. He shaved in the darkness in the bathroom, and returned repeatedly thereafter checking on imagined flaws on his face that he saw in the mirror. He literally got stuck in the mirror and the bathroom for hours on a daily basis. His social circle and connections began to get smaller. His social life slowly diminished. School became an issue. He would always overdo his assignments, not be able to live with anything less than perfection, and even be hard on himself for not knowing in advance what a teacher was going to teach him that day before s/he did. We had to withdraw him from formal schooling by his sophomore year in high school. The initial change in personality and in behavior came quickly at age 11 and then it was the unpredictable roller coaster ride up and down during the subsequent years as therapists, counselors, doctors, and we tried to understand what was going on with our dear boy/young man.
Q. Why do you think so few understand what BDD is? How would you explain it to someone who has never heard of it before?
A. BDD is poorly understood because it hadn’t been recognized as a disorder until the mid 1980s. Katharine Phillips put the brain disorder on the map with her famous book The Broken Mirror. Everything she described in the text, Nathaniel had and had experienced. Although the disorder label was publicly available, very few therapists recognized its behavioral manifestations in their patients. If you were tall and handsome and beautiful like Nathaniel, would you feel comfortable announcing to others that you were obsessed all day with unrelenting worries about your looks? Folks would think you were vain. So, in general, sufferers tend to say nothing. They simply suffer in silence. Unlike the other OCD-related disorders, BDD self-awareness is rather poor. We now know that a BDD sufferer has perceptional processing problems, which accounts for the distortions described above. Nevertheless, what a sufferer sees, s/he totally and truly believes to be true. It is difficult for that person to achieve any level of objectivity. It affects up to 2% of the population. That’s a high percentage rate, yet mention BDD to anyone on the street, and you get a blank stare in return. Nobody seems to know it. Given the high suicide rate in the rank of BDD sufferers, we have a fatal illness on our hands, in my opinion. Medication dosage administered is usually twice as high in BDD cases than for the other OCD-related illnesses. Effective treatment protocol needs to be slowly and methodically administered if the sufferer is to experience any kind of relief. Of course, there are various levels of BDD illness. In hindsight, I think Nathaniel had the worst case of it. Although we sought the help and advice of the best professionals in the field, Nathaniel’s BDD progressed. There were some moments of hope for healing along the way, but the relapses were cruel and drove him even further down into the pit of despair. He could not imagine growing old with this impossible illness, and adopting a lifestyle that would require regular medication, counseling and, perhaps even occasional in-patient treatment as a tune-up. For Nathaniel, this was not a life to live for!
Q. How is BDD related to OCD? Do they share any treatment methods, such as therapy or medication?
A. The obsessive behavior of BDD sufferers is similar to what we see in OCD. However, there are many differences. I do know that the SSRIs used in treatment for BDD are almost double in dosage for effective treatment than those used for regular OCD patients. Although there are day clinics and treatment programs specifically for BDD patients, those sufferers who need hospitalization or overnight surveillance are usually grouped with OCD-ers. Good BDD therapists would suggest that the treatment protocol be administered at a slower pace and that CBT treatment be more specifically tailored to this disorder. Of course, addressing the perceptional distortion remains key to healing. This would require visual retraining that works in tandem with the long-term behavioral restructuring required for control of unwanted thoughts.

Nathaniel
Q. Let’s pretend I’ve said the following to you: “The issue is that people today are just too caught up in material things and their looks. If they would just stop being so vain and focus on their inner beauty this wouldn’t be a problem.”
A. A BDD sufferer is anything but vain. H/she is a silent sufferer of his/her illness. The inner turmoil is constant and very unrelenting. Sufferers usually don’t dare to mention what’s on their mind 24/7. Why would they? No one would believe them based on what the observer sees. Reassurance given by others is only a temporary patch of relief. It never lasts long and only fuels the retched beast. Unfortunately, those who are rich and have the financial means have recourse to plastic surgery as a temporary solution to their angst. Unfortunately, those procedures only give temporary relief, if any. Think Michael Jackson — so many surgeries that eventually his whole face totally appeared distorted by those interventions. But he had the money to pay, and no doubt the plastic surgeons involved didn’t dare to question the patient’s motive to assess whether or not BDD was the root of the malaise. I’m so appreciative of Reid Ewing, the actor on ABC’s Modern Family, who recently came out and publicly announced that he suffers from BDD and that all the plastic surgeries he underwent did not help one bit. What is more worrisome, however, is that those same surgeons never dug deeper to discern whether or not he had BDD, a brain disorder. Now that’s really unprofessional behavior.
Q. It seems that people assume mostly women suffer from the disorder. Has anyone expressed surprise that your son had BDD?
A. Good question. I think statistically the number is practically 50/50. Women and our cultural focus on women and fashion would suggest that BDD be more evident among females. However, muscle dsymorphia with men is gaining greater recognition these days — men who focus on their bodies, their physical build, their muscles, and their general appearance and body proportions. Our culture of aggressive advertisement that celebrates bodily perfection does not help the BDD cause, for sure. However, it was interesting for me to learn that there are even cases of BDD in remote villages in Africa where such cultural distractions and focus are absence or negligible. Check out Argentina where plastic surgery for woman is now a cultural phenomenon. How an Argentinian woman looks and the public and private discourse about her weight and size are quite disturbing phenomena, in my opinion. The culture is indeed playing a role in nurturing BDD.
Q. What advice do you have for my younger readers who may be suffering in silence? How could a teenager approach his or her parents for support — and what if parents don’t understand and refuse to believe there’s a problem?
A. Don’t suffer in silence and in isolation! Find someone you can trust and describe what’s going on inside your head, even if it sounds a bit silly in the telling. Be sure you open up to someone who is non-judgmental and a really good listener. Let him/her know how painful your daily journey is. If possible, create a team dedicated and committed to your ultimate healing (parents, siblings, and even a good and close friend, etc.). Check out the new BDD website at IOCDF launched a year ago. There is something there for everyone — sufferer, parent, sibling, educator and professional. Invite your team to consult this rich resource too. Be sure your therapist/counselor/psychiatric/psychologist knows something about BDD and is well read and well trained in the treatment protocol. Strongly suggest that your family read the most recent literature about BDD, starting with Katharine Phillips’ book The Broken Mirror. Let them know that there are now specific treatment protocol manuals available, including one co-authored by Sabine Wilheim. But more importantly, try to understand that your brain is physically broken and that is why you are experiencing what you are experiencing. The bio-chemical process is physically responsible for the perceptional distortion. And don’t forget to add into the mix daily meditation, regular exercise, and good nutrition as ways to help support your efforts to heal. Let your personal mantra be, “I can do this. We can do this. I’m not alone. We are a team working together so I can heal. I deserve to be well and whole and complete in life!”

Denis and his wife, Judy
Q. How can people get involved in spreading awareness?
A. Getting the word out is not easy. If BDD affects 2% of the population, there is a good likelihood that someone in your life is impacted by this awful illness and is suffering immensely because of it on a daily basis. And worse still, no one knows! It is the personal story of one sufferer who did not deserve to suffer so cruelly. Let my awareness efforts inspire others to do something rather than feel victimized. Join the annual IOCDF 1,000,000 steps for OCD Awareness Walks in June. Can’t make it to Boston? Create your own awareness walk. No matter how small the team or the event, when you connect with other walkers physically or virtually, the community of supporters becomes larger and awareness grows incrementally, a step at a time. That is how all journeys begin and move forward. Moving forward beats staying still and stagnant. For me, it is definitely the ultimate balm for body, mind, spirit, and soul.
Q. If you could offer just one piece of advice to someone with OCD or BDD, what would it be?
A. Please seek help! And remember, you are not alone! There are folks out there who want to help and can!
(Alison Dotson is the author of Being Me with OCD: How I Learned to Obsess Less and Live My Life. She was diagnosed with OCD at age 26, after suffering from “taboo” obsessions for more than a decade. She is now the president of OCD Twin Cities, an affiliate of the International OCD Foundation, and has spoken about her experiences with OCD with several media outlets, including NBC, The Atlantic, Glamour, and The Huffington Post, as well as at national conferences.)
 1986 was a banner year, the year both our son, Nathaniel, and the International OCD Foundation came into existence. Unfortunately, Nathaniel died of one of the OCD-related disorders this organization fights so hard to overcome. And I’m also now on the Foundation’s Board of Directors supporting its mission “to help those afflicted with OCD and related disorders live full and productive lives.” Sadly, I was not able to attain that goal for my own son.
1986 was a banner year, the year both our son, Nathaniel, and the International OCD Foundation came into existence. Unfortunately, Nathaniel died of one of the OCD-related disorders this organization fights so hard to overcome. And I’m also now on the Foundation’s Board of Directors supporting its mission “to help those afflicted with OCD and related disorders live full and productive lives.” Sadly, I was not able to attain that goal for my own son. and young adolescence, to a robust adulthood of 30 quite successfully. The OCD Community has grown significantly both nationally and internationally over the years — good reason to celebrate.
and young adolescence, to a robust adulthood of 30 quite successfully. The OCD Community has grown significantly both nationally and internationally over the years — good reason to celebrate.